Counting excess vaccine donations as ODA inflated aid in 2021: Here's why they still shouldn't count
DI's Euan Ritchie explains how donors counted vaccines as ODA in 2021, and why the current OECD DAC rules on counting vaccines should change to stop inflating aid
In 2021, the OECD’s Development Assistance Committee (DAC) failed to agree on how to count donations of excess vaccine doses as ODA. Instead, they suggested a guideline price of US$6.72, and implemented ‘safeguards’ to satisfy those members who didn’t think excess vaccine donations should count as ODA at all. Now that full data for 2021 is available, this blog explores the differences in how donors reported, and finds that some of the safeguards were ignored and that a range of prices have been used. For 2022 data, it appears that a new, similar price (US$6.66) has been agreed. It would be simpler and more justifiable – and help to preserve the integrity of ODA – to exclude excess vaccine donations altogether, as some DAC members have argued for since the issue arose.
Donors failed to reach consensus on appropriate way to count vaccine donations
Officially, excess vaccine donations – vaccines donated to low- and middle-income countries that were not bought for that purpose but came from countries’ excess supply – were recorded at an average price of US$6.72 in 2021. However, this was a guideline price, as no consensus was reached on the appropriate way to count such donations as ODA. Hungary, which purchased and donated the more expensive Sinopharm vaccine (among others), refused to endorse the weighted average price of US$6.72, which therefore remained a guideline, and not formally binding.
Some countries agreed that excess vaccine donations could be counted as aid only reluctantly, on the condition that additional safeguards would be added. Notably, one such condition was reportedly that donations of excess vaccines from domestic supply would be eligible to count as ODA only in 2021 (after which time, donors should have been able to incorporate “vaccine procurement for low-income countries into regular development planning”, according to the US ).
Notwithstanding this condition, the DAC has apparently agreed to continue counting excess vaccine donations in the 2022 data at essentially the same price (US$0.06 lower than last year). This is despite some members reiterating the arguments against counting excess vaccine donations at all.
Not all countries followed the safeguards
Another important safeguard that was introduced to try and encourage skeptical donors to endorse the suggested rules was that in reporting such donations, donors should indicate “the vaccine names [and] number of doses” . For most countries, this information can be found in the OECD’s CRS dataset and provides welcome transparency around such donations. However, five countries – Ireland, the Republic of Korea, New Zealand, Poland and the UK – appear not to have adhered to this safeguard, reporting no information on either the type or total quantity of vaccines provided in the relevant CRS data fields.
Donors used a range of prices to count donations of excess vaccine doses as ODA
When the weighted-average price of US$6.72 was originally proposed , it appeared that it would allow some donors to ‘profit’ on their vaccine donations by counting more ODA per dose donated than they had originally paid (arguably, counting such donations as ODA at all inflates ODA numbers). For example, the UK had been planning to count donations at the DAC recommended price of US$6.72 despite having originally paid around US$2 less. To guard against this practice, the DAC secretariat adding the following clause to their guidelines:
For the sake of ODA integrity, members should verify the aggregate ODA figure reported for donations against their actual outlay in 2021 and make an adjustment if needed.
This rather ambiguous sentence is intended to ensure that countries use the guideline price only if it is lower than the average price paid for vaccines by the donor (it is not clear why the DAC did not state this explicitly). As Hungary shows, this is hardly binding, and in principle donors could still record higher prices than they paid, although many countries have ended up recording an average price lower than US$6.72. Czechia, for example, recorded an average of US$3.97 in ODA per donated dose. Despite initial fears of overcharging, it appears that the UK recorded an average price of around US$4.50 per dose (based on ODA recorded on excess vaccine donations of US$138 million, and reports that around 30 million vaccines were donated in 2021 — though the UK did not report this information in the CRS).
In addition, the US and the Netherlands opted not to report any ODA for their excess vaccine donations, given their principled objections to including them at all.
Figure 1: Average price at which excess vaccine dose donations were charged as ODA, 2021
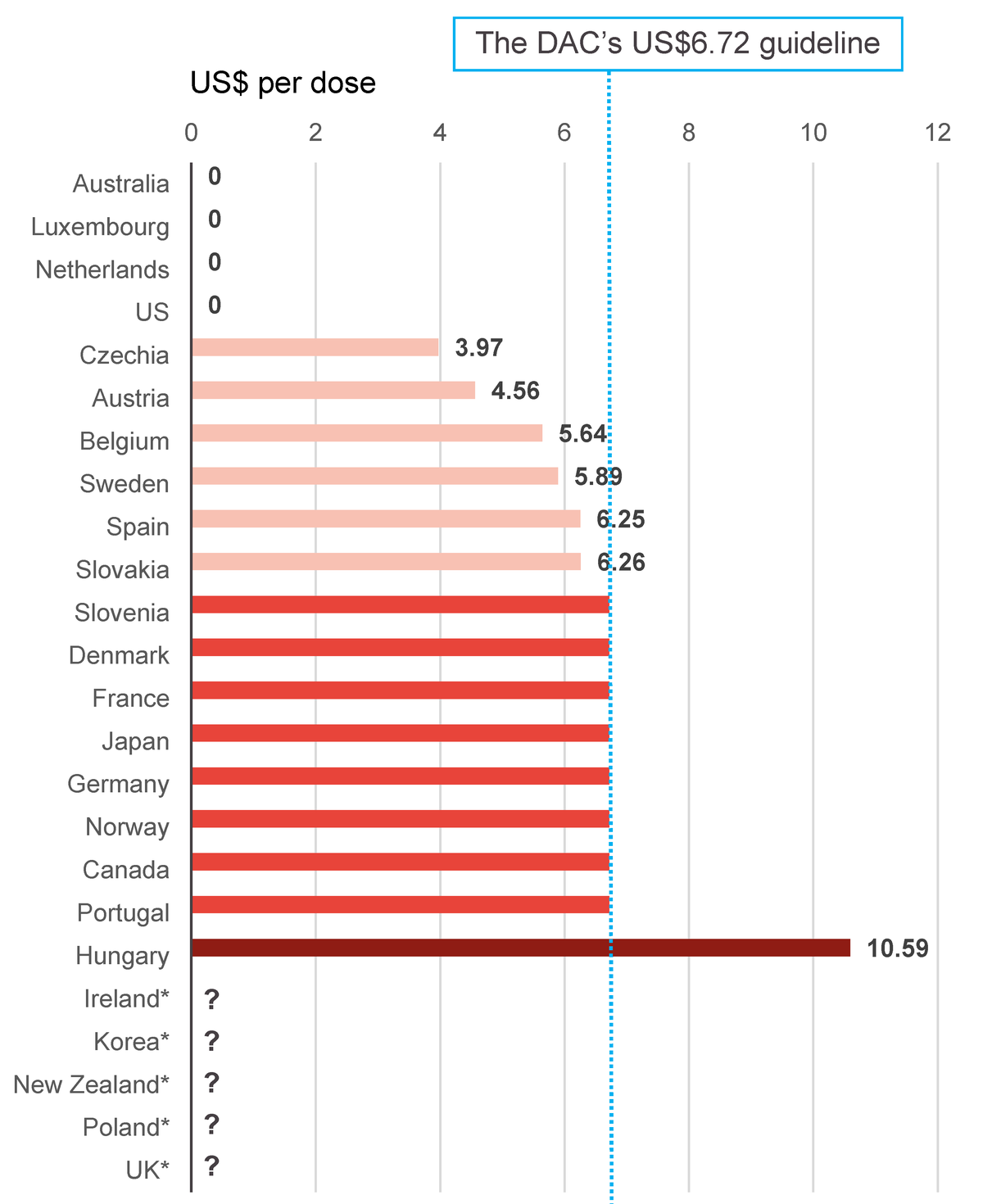
Bar chart showing the average price at which excess vaccine dose donations were charged as ODA in 2021 Australia, Luxembourg, the Netherlands and the US all charged US$0. The following countries charged less than the DAC’s guideline (which was US$6.72): Czechia (US$3.97), Austria (US$4.56), Belgium (US$5.64), Sweden (US$5.89), Spain (US$6.25), Slovakia (US$6.26) The following countries all charged the US$6.72 guideline: Slovenia, Denmark, France, Japan, Germany, Norway, Canada and Portugal. Hungary charged US$10.59 – above the guideline. The Republic of Korea, Ireland, New Zealand, Poland and the UK did not provide data.
Notes: Ireland, Republic of Korea, New Zealand, Poland and the UK all reported excess vaccine donations, but did not report sufficient information to determine an average price in the CRS data. The Netherlands and the US donated vaccines, but opted not to report ODA on these transactions.
Source: DI Analysis of OECD-CRS
The information raises interesting questions about the disparity between prices paid for vaccines between donors. For example, Czechia, Belgium and Hungary each recorded around US$2.10 in ODA per dose of the Oxford–AstraZeneca Vaxzevria vaccine, according to CRS data. While Japan donated only AstraZeneca vaccines, it used the average price of US$6.72, implying that either it ignored the safeguard noted above (adjusting prices to reflect actual outlays), or it paid more than three times as much as European countries (and considerably more than any other country according to the UN’s COVID-19 market dashboard ). If the former, it undermines the DAC’s attempt to prevent ODA inflation. If the latter, it highlights that including donations of excess vaccinations in ODA essentially makes ODA figures dependent on countries’ negotiations with pharmaceutical companies.
Ethical and practical arguments suggest continuing to count such donations is wrong
The DAC members advocating for removing excess vaccine donations as ODA are right, as they were last year. It’s hard to police all of the safeguards deemed necessary for full transparency. Vaccine types are so different, and their prices so negotiable, that there will never be a ‘market price’ that can be used as a common benchmark. And more importantly, the doses weren’t bought with development purposes in mind, and over-purchasing by donor countries contributed to vaccine inequality. Self-interest reasons alone should’ve been enough to induce countries to give away vaccines that they couldn’t possibly have used themselves anyway. This year, opponents to preserving inclusion point to another valid argument : 2021 was an exceptional year, and donors had been unable to incorporate vaccine procurement into their development planning. That’s no longer the case.
As DI has discussed elsewhere, how we measure aid matters . While the DAC secretariat has managed to prevent the worst fears of some commentators, by persuading members not to count more ODA per dose than they originally paid, it’s still true that including excess vaccine donations in ODA inflates the figures. With continuing criticism of the way the DAC operates, the decision to allow members to continue to record excess vaccine donations in 2022 – reneging on reassurances apparently made to some members – is an unnecessary own-goal.
This blog is part of a Development Initiatives series on debates concerning the rules for measuring official development assistance (ODA) , and potential reforms to its governing body, the Development Assistance Committee. ODA is the most widely used statistic on international aid, and how we measure it matters .
Related content
The DAC debates: why aid measurement matters for development
The way we measure aid affects the type and quantity provided as well as our perceptions of it. Why are the DAC's rules controversial?
Aid in 2021: Key facts about official development assistance
Our factsheet highlights key analysis of global aid reported in 2021. It includes the latest DAC data on providers, recipients, sectors and climate targeting.
How is aid changing in the Covid-19 pandemic?
This briefing sets out near real-time data on aid for the first half of 2020. It shows how commitments are changing in the Covid-19 pandemic and where these are most likely to affect the poorest people and places.